I’m realizing how much of a bubble I’ve been living in in the last 3 years.
Just as the pandemic was first spreading to the United States, I happened to be starting a job. I was a medical officer at Caremore and Aspire’s new Home Based Complex Care program. This was an incredible deep dive into the world of Medicare Advantage centric, “full risk” value-based primary care models. I dove even deeper in my next job as a medical director at Clover Health’s very similar In-home Complex Care program.
During this time, I lived in the insular world of “primary care for medicare advantage”. These sorts of companies have been making the news lately due to insanely high valuations that mega-corporations have been willing to pay for them. Prime (no pun intended) examples include:
Iora Primary Care , which is the piece of One Medical that Amazon may have been most interested in during the $3.8 Billion acquisition
Landmark Health the nation’s leading home visiting focused version of these models, acquired by United Healthcare for an estimated $3.5 Billion
Oak Street Health, purchased for a jaw-dropping $10 Billion with a B by CVS
Even ChenMed, the OG of medicare advantage focused fully risk primary care models, is now rumored to be on Walmart’s buy list
To understand this corporate obsession, you need to look at the same graphs on expansion of Medicare Advantage these corporate M&A teams look at. The total number of Medicare beneficiaries is increasing rapidly. Notice that the buyers are all either mega-retailers, that I’m assuming are looking to hook boomers’ other purchasing habits (Amazon and Walmart), or insurers with a heavy MA heavy strategy (CVS/Atena and United).
The number of Medicare Advantage enrollees number go up!
Buy! Buy! Buy!
Inside the world of Medicare Advantage, care coordination heavy primary care is a no brainer. All the models above rely heavily on nursing and social work led care management. Those models live and die by keeping the total cost of care down, and that essentially translates to preventing avoidable hospitalizations. The most effective way to do that is care management. I used to describe the work our disciplinary teams did when I was in this world as “care management with some primary care medicine sprinkled on top”. It makes sense in full risk MA models to invest heavily in care management.
To those of you practicing or working in the more typical Fee For Service (FFS) world this might sound like a magical fairy land, but it exists and it works (although I have my concerns about this model applied at scale, especially now that mega corps like Amazon are in the mix). To me, having lived here for the last 3 years, and been deeply involved in this world since fellowship, it feels like home.
I’ve been taken up in the tornado of healthtech bubble market chaos, and dropped off in a new land. Let’s call it FFS Oz. To everyone else in medicine this land feels normal. In FFS Oz, billing for procedures and encounters, waiting for patients to follow-up with you rather than the other way round, and very little to none of your day looking at panel-wide data to understand trends and risks is normal. To me, that’s no way to practice medicine. FFS is stuck in an encounter-centric world, that makes no sense when most serious disease today is chronic and deeply related to lifestyle and social determinants of health. Is the world I came from an illusionary Emerald City?
In FFS, it doesn’t seem like there is any yellow brick road towards this Emerald City of high functioning practice model, led by care management, focused on populations, and utilizing creative models of care delivery like remote-patient monitoring and home visits.
Yet, find the Emerald City we must. Medicare Advantage (MA) is still only 50% of Medicare beneficiaries, and in some regions, like Chester and Montgomery counties in Pennsylvania where I am, less than 40% of Medicare enrollees chose MA. Medicare Advantage enrollment seems to have quite a but of regional variance (with urban areas more concentrated in MA than rural communities). The vast majority of primary care providers and community physicians cannot and should not take on risk (insurance companies with legions of actuaries and legally obligated massive capital reserves offsetting their risk to small, thin-margined primary care doctors never really made much sense to me). So
There are still millions of Medicare beneficiaries that are not on an MA plan.
Who will coordinate and manage their care?
When I left the Unicorn trodden land of closely aligned, full risk bearing primary care for MA, to return to the private practice solo doctor shingle hanging medicine, I realized I am not in Kansas anymore.
(Note: The actual Kansas has very low Medicare Advantage penetrance. I’m obviously referring to the proverbial Kansas. This Oz analogy is getting old, but let’s try once more.)
The yellow brick road to the Emerald City of sustainable medical practice that focused on populations and care coordination is possible. It seems to be the new CMS fee- for-service Medicare codes might be these yellow bricks for a solo straight-medicare accepting FFS practice primary care practice. What are these new(-ish) Medicare codes for FFS practice that I speak of. The loose conglomeration of procedure codes that pay practices for doing care coordination without a physician visit needing to be the center of their financial universe.
CCM, TCM, and RPM, oh my!
(There I did it! Awful Oz analogy complete!)
(Prompt for image: “Dorothy from Wizard of Oz as a nurse care manager”. )
These codes, from my perspective of imaging how to build a high quality primary care practice serving older adults with complex chronic conditions, seem like the perfect opportunity. In a normal FFS primary care practice, I live and die by the E/M encounter. There is very little reason, from a financial perspective, to have staff follow up with the patients on the recommendations I as a doctor made.
Having a nurse or other trained staff call and ask “Did you get your screening test done?”, “Did you meet with the nutritionist?”, “How you doing with understanding how to take your diabetes medications?”, and track those activities, and assist the patient in getting those things done, is medically the right thing to do. Yet if my practice’s financial model is entirely dependent on me the doctor just getting in the room to see the next patient, then this labor and technology intensive (you need specialized software to track all this and very few good ones for this exist on the market yet) process is simply a cost that my thin-margin practice can’t afford.
But, if a major financial driver of my practice is care management itself, i.e. Medicare is literally paying me and my staff to do good follow-up and care management, its a complete game changer. Now, this labor and technology is not a cost center, but a revenue driver! Now hiring, training, and technologically equipping a large staff to do this important work well makes it financially sustainable to do this work well. Not just financially sustainable. With the newer high reimbursement rates CMS announced in 2022 , providing this service should be quite lucrative! Not only that, the evidence is strong that patients who receive the CCM service, in claims analysis, have fewer avoidable hospitalization and ED visits. Patients seem satisfied with the service.
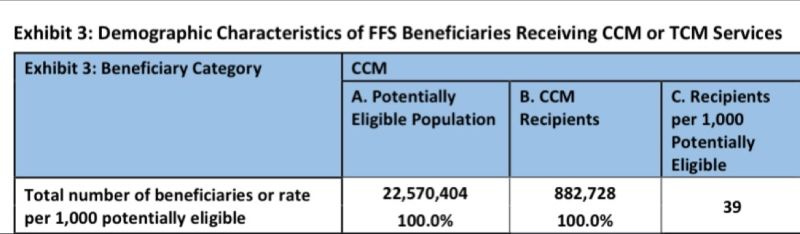
Yet, uptake among primary care doctors, is slow. Less than 4% (39/1000) of eligible Medicare beneficiaries are receiving the care?
This is particularly true among small primary care practices in rural communities that have been the slowest to uptake these codes, even though this is where it seems like patients (and the practices that serve them) would benefit most.
On LinkedIn the other day, I asked why more primary care doctors aren’t offering this service. Very knowledgable people shared a wide range of answers, and there are a variety of good reasons why uptake is so low. A future article here will dig deeper into this topic. Yet, nothing I have found is convincing that a primary care practice shouldn’t heavily build around being able to provide reliably the services supported by these codes. This is especially if you are building from the ground up.
To me, CMS’s support, with real dollars, of these unique codes that capture the important work of primary care that happens outside the “E/M” encounter, is an opportunity for innovative primary care doctors to build entirely new models of care, without having to take un the unsustainable down-side financial risk of a “full risk” contract with a Medicare Advantage plan. There may be something I am missing, but it is worth exploring.
Ready, Toto? We’re not in Kansas anymore. Its time to follow the yellow brick road!
(Couldn’t help myself.)